Table of Contents
Wechseljahre Symptome verstehen: Lerne auf deinen Körper in der Lebensmitte zu hören
This page may contain affiliate links. We may earn a commission on purchases, at no additional cost to you. Learn more →
Geschrieben von Dr. Cathleen Brown , staatlich geprüfte Gynäkologin.
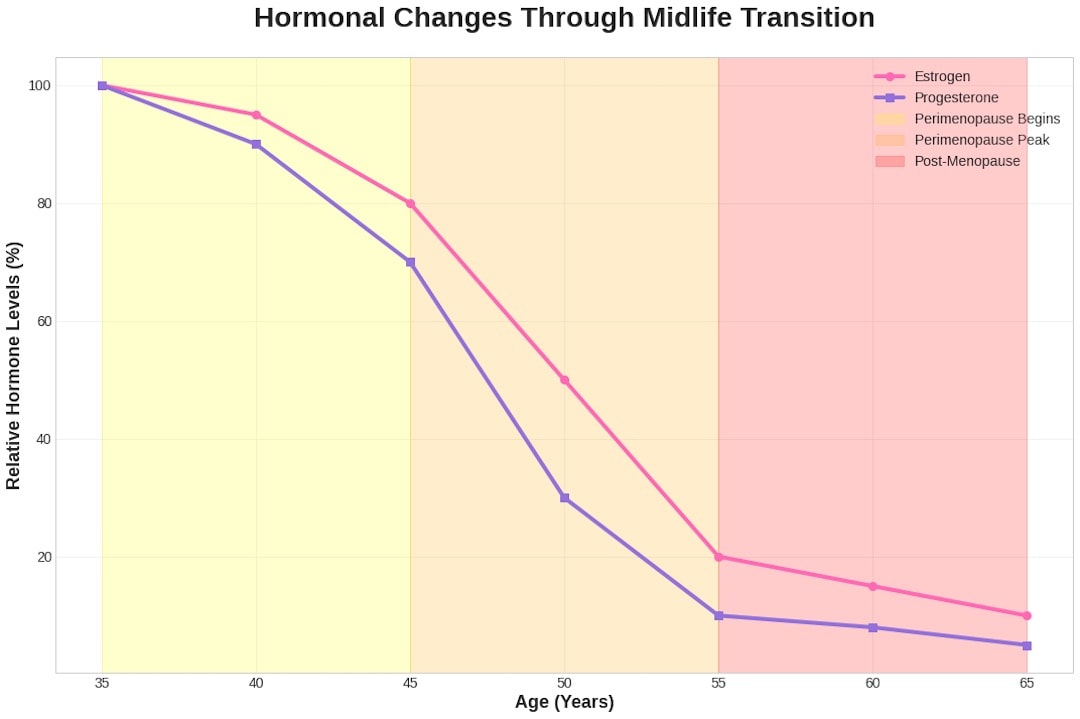
Die Lebensmitte kommt nicht mit einer Gebrauchsanweisung daher; oft schleicht sie sich leise ein und beginnt allmählich umzuschreiben, wie dein Körper reagiert. Diese Übergangsphase im Leben – oft Perimenopause genannt – erstreckt sich typischerweise über die 40er und 50er Jahre einer Frau und bringt bedeutende hormonelle Veränderungen mit sich, die nahezu jedes Körpersystem beeinflussen.
Während dieser Zeit schwanken die Hormone stark, was zu einer Vielzahl von Wechseljahresbeschwerden führt, wie Hitzewallungen, nächtlichen Schweißausbrüchen, Stimmungsschwankungen und Scheidentrockenheit. Speisen, die früher problemlos verdaut wurden, können sich jetzt schwer anfühlen, Erholung stellt sich möglicherweise nicht mehr mit der gewohnten Zuverlässigkeit ein, und Gefühle können auf unbekannte Art und Weise an die Oberfläche kommen.
Diese Veränderungen sind nicht nur lästige Symptome der Wechseljahre; sie sind tiefgreifende Botschaften eines Körpers, der eine natürliche Umstellung durchläuft. Auf deinen Körper zu hören wird in dieser Phase weniger zu einer Frage des "Reparierens" und mehr zu einer Frage des tiefen Verstehens und der Pflege einer Partnerschaft.
Tiefes Zuhören ohne Vorurteile ermöglicht Anpassungen, die Widerstandsfähigkeit, Wohlbefinden und die allgemeine Lebensqualität unterstützen. Diese Anpassungen werden körperlich, zutiefst persönlich und emotional. Da dein Körper mehr in Nuancen als in Lautstärke kommuniziert, ist es nicht deine Aufgabe, ihn zu disziplinieren, sondern mit ihm zusammenzuarbeiten und seine angeborene Intelligenz und Weisheit anzuerkennen.
Was kannst du also tun, um diesen Übergang in der Lebensmitte zu meistern? Im Folgenden erkunden wir wichtige Bereiche der Frauengesundheit, die von der Perimenopause betroffen sind – von ausreichender Flüssigkeitszufuhr und besserem Schlaf bis hin zur Pflege der sexuellen Gesundheit, Kraft, Haut, emotionalen Balance, Verdauung und sogar deines Selbstverständnisses. Jeder Abschnitt bietet Einblicke und praktische Tipps, um dir zu helfen, die "Weisheitsflüstern" deines Körpers während der Wechseljahre zu würdigen.
Flüssigkeitszufuhr & Hitzewallungen in der Perimenopause
Ausreichende Flüssigkeitszufuhr ist ein grundlegendes Fundament der Gesundheit, das während der Wechseljahre noch wichtiger wird. Östrogen spielt eine entscheidende Rolle bei der Flüssigkeitsbalance, und wenn seine Werte während der Perimenopause und Menopause schwanken und abnehmen, verändert sich die Fähigkeit des Körpers, Feuchtigkeit zu speichern und zu regulieren. Das wirkt sich auf verschiedene Systeme aus, von der Gehirnfunktion bis hin zur Gelenkgesundheit. Während manche Frauen ein verringertes Durstgefühl verspüren, können hormonelle Veränderungen auch zu verstärktem Durst führen, obwohl Symptome wie trockene Haut und Augen möglicherweise deutlicher wahrnehmbar sind. Viele Frauen in den Wechseljahren beschreiben anhaltende Trockenheit – Haut, die sich nach dem Waschen gespannt anfühlt, Augen, die schneller ermüden, oder Lippen, die leicht einreißen. Das sind körperliche Anzeichen verringerter Wasserspeicherung und veränderter Flüssigkeitsverteilung, verursacht durch niedrigere Östrogenwerte, die den Blutfluss und die feuchtigkeitsspendenden Moleküle im Gewebe beeinflussen.
Häufige Anzeichen von Flüssigkeitsmangel in der Lebensmitte sind:
-
Trockene oder schuppige Haut (Haut kann sich gespannt, juckend anfühlen oder stumpf aussehen)
-
Häufige Kopfschmerzen am Nachmittag
-
Verringerte Urinmenge oder dunklerer Urin (ein Zeichen dafür, dass du mehr Flüssigkeit brauchst)
-
Verstärkte Muskelkrämpfe oder Muskelermüdung
-
Stimmungstiefs und Reizbarkeit
-
Nebelige Gedanken oder Konzentrationsschwierigkeiten
Schon leichte Dehydrierung kann nachweislich Gedächtnis, Konzentration und Stimmung beeinträchtigen, was die entscheidende Verbindung zwischen Flüssigkeitshaushalt und kognitiver Funktion unterstreicht. Während sich der Körper anpasst, können Symptome wie Hitzewallungen und Schweißausbrüche zu verstärktem Flüssigkeitsverlust führen, wodurch eine gleichmäßige Flüssigkeitszufuhr für die Temperaturregulierung noch wichtiger wird.
Sinkendes Östrogen wirkt sich auch auf Knorpel und Gelenkschmierung aus; ausreichende Flüssigkeitszufuhr kann helfen, Steifheit und Beschwerden zu reduzieren. Die Flüssigkeitszufuhr unterstützt auch die Vaginalgesundheit, indem sie dabei hilft, die Feuchtigkeit der Schleimhäute aufrechtzuerhalten und Trockenheit sowie Beschwerden im Zusammenhang mit niedrigeren Östrogenspiegeln zu lindern.
Es geht nicht nur um das Wasser selbst – Elektrolyte (Mineralien wie Natrium, Kalium, Kalzium und Magnesium) sind entscheidend für die Aufrechterhaltung der Flüssigkeitsbalance und helfen deinem Körper dabei, Wasser effektiv zu absorbieren. Progesteron, ein weiteres Hormon, das in der Lebensmitte absinkt, kann wie ein Diuretikum wirken (wodurch du mehr Wasser und Elektrolyte verlierst). Daher ist es wichtig, genügend Elektrolyte über die Ernährung oder Nahrungsergänzungsmittel aufzunehmen, besonders wenn du durch Hitzewallungen stark schwitzt.
Tipps für ausreichende Flüssigkeitszufuhr: Versuche, die Flüssigkeitszufuhr in deinen Alltag zu integrieren. Beginne zum Beispiel den Morgen mit einem Glas Wasser oder Kräutertee, trinke zwischen den Aufgaben kleine Schlucke und baue wasserreiche Lebensmittel in deine Ernährung ein (Gurken, Beeren, Zitrusfrüchte, Blattgemüse usw.). Eine allgemeine Richtlinie ist, etwa 2–3 Liter Flüssigkeit pro Tag anzustreben, aber höre auf deinen Körper – du könntest mehr brauchen, wenn du sehr aktiv bist, in einem warmen Klima lebst oder häufig Hitzewallungen und Schweißausbrüche hast. Eine einfache Methode, um deinen Flüssigkeitshaushalt zu überprüfen, ist die Kontrolle der Urinfarbe: Wenn er dunkelgelb ist, ist das ein Zeichen dafür, dass du mehr trinken solltest.
Baue auch elektrolytreiche Lebensmittel ein (wie Bananen für Kalium oder Nüsse und Samen für Magnesium und Kalzium) oder denke über ein ausgewogenes Elektrolytgetränk oder -supplement nach, besonders während Phasen starken Schwitzens. Achte auf Getränke, die dich dehydrieren können – versuche übermäßigen Koffein- und Alkoholkonsum zu begrenzen, da sie dazu führen, dass du mehr Flüssigkeit verlierst. Wenn du deine Flüssigkeitszufuhr konstant hältst, wirst du oft Vorteile bemerken, die über das Stillen des Durstes hinausgehen: stabilere Energieniveaus, bessere Verdauung, klareres Denken und eine insgesamt bessere Fähigkeit deines Körpers, mit hormonellen Schwankungen umzugehen. Betrachte die Flüssigkeitszufuhr als grundlegenden Teil deines Wellness-Werkzeugkastens für die Wechseljahre – es ist eine einfache, aber kraftvolle Art, deine körperliche und sogar emotionale Gesundheit zu unterstützen.
Schlafstörungen in der Lebensmitte (Perimenopause-Schlaflosigkeit)
Schlafstörungen in der Lebensmitte sind ein weit verbreitetes Problem, das 40% bis 61% der Frauen betrifft. Diese Störungen entstehen nicht immer nur durch schlechte Gewohnheiten; hormonelle Veränderungen, insbesondere bei Östrogen und Progesteron, wirken sich direkt auf die Schlafarchitektur und die regulierenden Systeme aus. Progesteron, das "entspannende Hormon", trägt zu Einschlafproblemen bei, wenn es abnimmt. Östrogen beeinflusst den Stoffwechsel von Neurotransmittern wie Serotonin und Melatonin, die für die Regulierung des zirkadianen Rhythmus und der Schlafmuster entscheidend sind. Es spielt auch eine Rolle bei der Temperaturregulierung.
Viele Frauen in den Wechseljahren bemerken ein Muster, bei dem sie jede Nacht zur gleichen Zeit aufwachen – häufig gegen 3 Uhr morgens. Manchmal wird das durch nächtliche Schweißausbrüche oder Hitzewallungen ausgelöst, die dich plötzlich heiß und hellwach werden lassen. Andere erleben sehr lebhafte Träume oder finden sich einfach mitten in der Nacht ohne ersichtlichen Grund hellwach wieder. Diese Schlafprobleme sind mehr als nur lästige Störungen; sie sind Signale dafür, dass sich die innere Umgebung deines Körpers verändert und möglicherweise Unterstützung braucht. Das Älterwerden im Allgemeinen, Veränderungen der Stresshormone und Stimmungsstörungen (die in der Lebensmitte auftreten oder sich verschlimmern können) können ebenfalls eine Rolle bei Schlafproblemen spielen.

Tipps für besseren Schlaf in der Lebensmitte
Es ist hilfreich, eine Schlafumgebung und -routine zu schaffen, die die Grundlage für erholsamen Schlaf bildet:
-
Halte das Schlafzimmer kühl und komfortabel: Viele Experten empfehlen etwa 18°C als ideale Schlaftemperatur. Ein kühlerer Raum kann helfen, Hitzewallungen und nächtlichen Schweißausbrüchen entgegenzuwirken. Verwende atmungsaktive, feuchtigkeitsableitende Schlafanzüge und mehrschichtige Bettwäsche, die du leicht anpassen kannst, wenn dir zu warm wird.
-
Etabliere eine beruhigende Abendroutine: Erwäge die Einnahme von Magnesium (wie Magnesiumglycinat) am Abend, falls angemessen – Magnesium kann Entspannung fördern. Genieße eine Tasse beruhigenden Kräutertee wie Melisse oder Rooibos. Das Dimmen der Lichter und Ausschalten der Bildschirme mindestens eine Stunde vor dem Schlafengehen kann deinen Körper dazu ermutigen, Melatonin zu produzieren und deinem Geist beim Entspannen helfen.
-
Praktiziere Entspannungstechniken: Sanfte Yoga-Dehnungen, tiefe Atemübungen oder eine Körper-Scan-Meditation vor dem Schlafengehen können die "Kampf-oder-Flucht"-Stressreaktion reduzieren, die dich möglicherweise wach hält. Das Führen eines Tagebuchs vor dem Schlafengehen ist eine weitere großartige Gewohnheit – es hilft dabei, kreisende Gedanken zu externalisieren, geistiges Geplapper zu beruhigen und die mentale Gesundheit zu verbessern.
-
Achte auf deine Abendernährung und -gewohnheiten: Versuche Koffein am späten Nachmittag und Abend zu vermeiden, ebenso wie Alkohol oder Nikotin kurz vor dem Schlafengehen – all diese können die Schlafqualität stören. Wenn nächtliche Hitzewallungen ein Problem sind, sei vorsichtig mit scharfen Speisen oder schweren Mahlzeiten am Abend, da diese Beschwerden auslösen können. Auch wenn ausreichende Flüssigkeitszufuhr wichtig ist, möchtest du vielleicht die Flüssigkeitsaufnahme ein bis zwei Stunden vor dem Schlafengehen reduzieren, damit du nicht so oft für Toilettengänge aufwachst.
Denke daran, dass das Finden der richtigen Schlafstrategie etwas Ausprobieren erfordern kann. Wenn Schlaflosigkeit oder gestörter Schlaf anhält und dein Leben erheblich beeinträchtigt, solltest du mit einem Arzt oder einer Ärztin sprechen. Sie könnten Lösungen wie kognitive Verhaltenstherapie bei Schlaflosigkeit oder sogar eine Hormonersatztherapie empfehlen. Eine Hormonersatztherapie kann für manche Frauen den Schlaf verbessern, indem sie die Hormonspiegel stabilisiert und nächtliche Schweißausbrüche sowie Hitzewallungen, die den Schlaf stören, erheblich reduziert. Erholsamen Schlaf zu bekommen ist kein Luxus – er ist essentiell für deine Stimmung, kognitive Funktion und körperliche Gesundheit während des Übergangs in der Lebensmitte.

Sexuelle Gesundheit & Intime Beschwerden: Auf die leisen Signale des Körpers hören
Sexuelle Gesundheit ist ein wichtiger Bestandteil der Frauengesundheit in der Lebensmitte, doch es ist ein Bereich, in dem viele Frauen während der Wechseljahre Herausforderungen erleben.
Sexuelle Funktionsstörungen – einschließlich Scheidentrockenheit, verminderter Libido und Schmerzen beim Geschlechtsverkehr – sind häufige, aber oft nicht angesprochene Symptome der Wechseljahre. Diese Beschwerden können Intimität und Selbstwertgefühl beeinträchtigen, aber es gibt wirksame Lösungen.
Der Rückgang des Östrogens in der Lebensmitte verursacht körperliche Veränderungen in den Geweben der Vulva, Vagina, Harnröhre und Blase. Zusammenfassend werden diese Veränderungen als urogenitales Syndrom der Menopause (GSM) bezeichnet. Östrogen ist entscheidend dafür, diese Gewebe dick, elastisch, gut durchblutet und natürlich befeuchtet zu halten. Wenn die Östrogenspiegel sinken:
-
Die Vaginal- und Vulvagewebe werden dünner, trockener und weniger elastisch.
-
Die Durchblutung des Genitalbereichs nimmt ab.
-
Die natürliche Befeuchtung reduziert sich.
-
Das Harnröhren- und Blasengewebe kann ebenfalls dünner und brüchiger werden.
Dies führt zu Symptomen wie Trockenheit, Juckreiz, Brennen, Reizungen und Beschwerden oder Schmerzen beim Geschlechtsverkehr. Veränderungen im Harnröhren- und Blasengewebe können auch zu verstärktem Harndrang, häufigem Wasserlassen oder wiederkehrenden Harnwegsinfektionen führen. Diese Symptome sind nicht geringfügig; sie können körperliches Wohlbefinden, Selbstwertgefühl und Beziehungen tiefgreifend beeinträchtigen.
Wenn du auf Empfindungen während der Bewegung oder täglichen Hygienroutinen achtest, offenbaren sich subtile Anzeichen dieser Gewebeveränderungen. Eine neue Empfindlichkeit gegenüber bestimmten Waschmitteln oder Badeprodukten oder Beschwerden beim längeren Sitzen können auf Gewebeveränderungen hinweisen, die Unterstützung benötigen.
Tipps zur Wiederherstellung von Komfort und sexueller Gesundheit:
Es gibt verschiedene Ansätze, um Scheidentrockenheit und andere GSM-Symptome zu lindern, und oft funktioniert eine Kombination am besten:
-
Atmungsaktive Unterwäsche aus Bio-Baumwolle hilft dabei, Reizungen zu reduzieren und die Luftzirkulation zu verbessern.
-
Wasser- oder silikonbasierte Gleitmittel mit sauberen Inhaltsstoffen verbessern den Komfort beim Geschlechtsverkehr erheblich.
-
Regelmäßige Anwendung von Vaginalfeuchtigkeitscremes (unterscheiden sich von Gleitmitteln) befeuchtet das Gewebe und verbessert die Elastizität.
-
Sanfte Beckenboden-Dehnungen oder Beckenboden-Physiotherapie helfen dabei, die Durchblutung zu verbessern, Muskelverspannungen zu reduzieren und Beschwerden zu lindern.
-
Sitzbäder mit beruhigenden Inhaltsstoffen wie Ringelblume oder Kamille können entspannende Eigenschaften haben.
-
Hormonersatztherapie und andere medizinische Optionen können von einem Arzt oder einer Ärztin empfohlen werden.
Diese Lösungen respektieren die zugrundeliegende Physiologie. Offene Kommunikation mit medizinischen Fachkräften über intime Gesundheitsprobleme ist entscheidend für angemessene Diagnosen und Behandlungspläne.

Bewegung: Kraft zurückgewinnen
Die Körperzusammensetzung verändert sich in der Lebensmitte nachteilig, beeinflusst durch sinkendes Östrogen. Der Muskeltonus verändert sich, mit einer Tendenz, magere Muskelmasse zu verlieren und Fett zuzunehmen, besonders Bauchfett, selbst ohne Gewichtsveränderung. Diese beschleunigte Fettzunahme und der Muskelverlust sind stark mit der Menopause verbunden. Diese Veränderung ist nicht nur ästhetischer Natur; sie hat stoffwechselbedingte Auswirkungen, einschließlich einer verlangsamten Stoffwechselrate, und erhöhtes Bauchfett ist mit einem erhöhten Risiko für chronische Erkrankungen wie Herz-Kreislauf-Erkrankungen und Diabetes verbunden.
Auf deinen Körper zu hören bedeutet hier weniger bestrafende Workouts und mehr intelligente Erhaltung und sanfte Stärkung. Bewegung wird zu einem Dialog mit deinen Gelenken, deiner Haltung und deinem Atem. Krafttraining ein paar Mal pro Woche ist entscheidend für die Erhaltung von Muskelmasse und Kraft und unterstützt die Knochengesundheit, da die Knochendichte mit dem Östrogenverlust rapide abnimmt. Gewichtstragende Übungen regen die Knochenbildung an. Spazierengehen oder Wandern bleibt ausgezeichnet für die Herz-Kreislauf-Gesundheit, Stimmung und Verdauung. An manchen Tagen sind nur sanfte Dehnungen nötig, um die Flexibilität zu erhalten und Verspannungen zu lösen.
Die besten Übungen für die Lebensmitte umfassen eine Reihe von Vorteilen:
-
Spazierengehen oder Wandern: Bietet Herz-Kreislauf-Vorteile, unterstützt Stimmung und Verdauung und ist gewichtstragend.
-
Krafttraining: Essentiell für die Erhaltung magerer Muskelmasse, Ankurbelung des Stoffwechsels und Aufrechterhaltung der Knochendichte. Kann Gewichte, Widerstandsbänder oder Körpergewicht beinhalten.
-
Sanftes Yoga: Verbessert Flexibilität, Balance, reduziert Stress und kann den Beckenboden unterstützen.
-
Pilates: Konzentriert sich auf Rumpfkraft, Flexibilität und Haltung, mit Schwerpunkt auf dem Beckenboden.
-
Gleichgewichtsübungen: Zunehmend wichtig für die Verletzungsprävention. Beispiele sind das Stehen auf einem Bein oder das Praktizieren von Tai Chi.
Darauf zu hören, wann sich der Körper durch Aktivität erschöpft oder belebt fühlt, hilft dabei, die richtige Dosierung und Art der Bewegung zu bestimmen. Finde Aktivitäten, die Spaß machen und nachhaltig sind. Das Aufschreiben, wie du dich vor und nach körperlicher Aktivität fühlst, zeigt auf, was ein normaler Teil des Kraftaufbaus ist versus Signale von Überanstrengung oder Ruhebedürfnis. Das Ziel ist es, Vertrauen in die Widerstandsfähigkeit deines Körpers zu entwickeln, nicht nur das Aussehen zu kontrollieren. Regelmäßige Aktivität hilft dabei, Gewichtszunahme und nachteilige Veränderungen der Körperzusammensetzung zu mildern.
Haut und Haare: Oberflächliche Signale
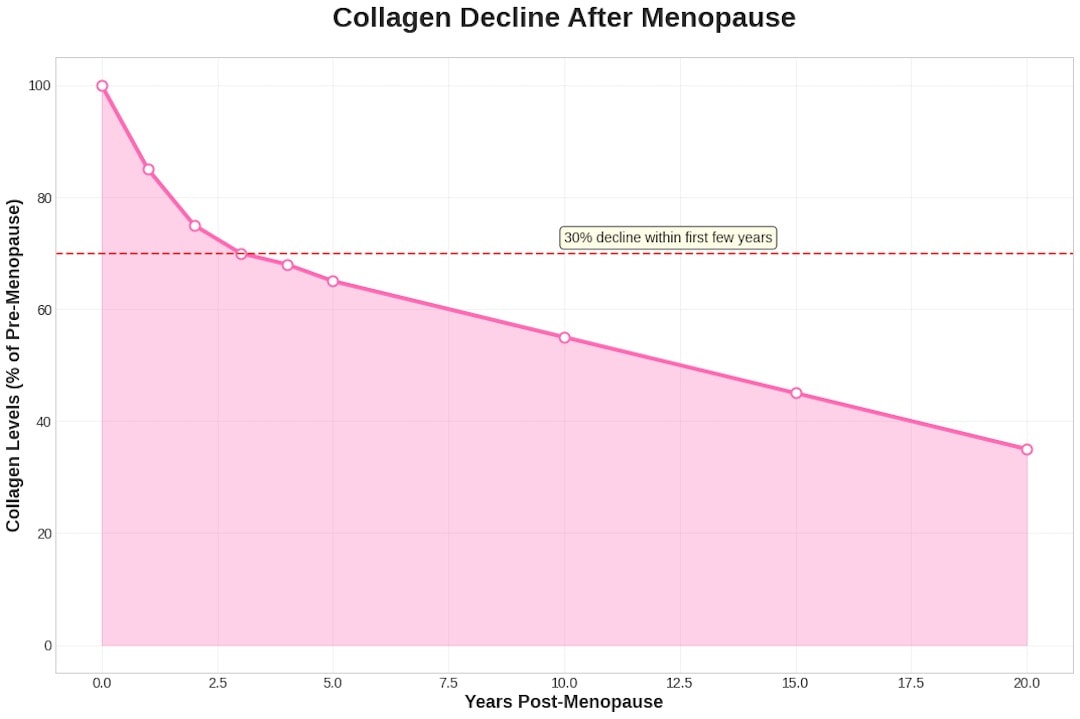
Veränderungen der Haut und Haare sind oft sichtbare Anzeichen der hormonellen Umstellung in der Lebensmitte. Sinkendes Östrogen wirkt sich erheblich auf die Haut aus. Östrogen ist entscheidend für die Erhaltung der Hautgesundheit, indem es die Kollagen- und Elastinproduktion anregt und so strukturelle Unterstützung, Elastizität und Festigkeit bietet. Es beeinflusst auch die Durchblutung, Talgproduktion und Hyaluronsäure, die der Haut hilft, Feuchtigkeit zu speichern.
Wenn die Östrogenspiegel sinken, besonders schnell nach der Menopause, gibt es eine erhebliche Abnahme von Kollagen (etwa 30%) und einen Verlust von Elastin. Das verdünnt die Haut, macht sie weniger elastisch und anfälliger für Erschlaffung, Falten und leichtere Blutergüsse oder Risse. Reduzierte Durchblutung, verminderte Talgproduktion und verringerte Hyaluronsäure tragen zu verstärkter Trockenheit, Schuppigkeit, Juckreiz und einer beeinträchtigten Hautbarriere bei, wodurch die Haut anfälliger für Reizstoffe wird. Diese Veränderungen können bereits während der Perimenopause beginnen.
Die Haarstruktur kann sich verändern und trockener oder brüchiger werden, und verstärkter Haarausfall oder dünner werdendes Haar ist häufig. Während hormonelle Schwankungen die Hauptverursacher sind, spielt auch der Nährstoffstatus eine Rolle. Biotin, Eisen und Omega-3-Fettsäuren werden oft diskutiert, aber die Verbindung ist komplex. Plötzliche oder übermäßige Haarveränderungen können eine ärztliche Untersuchung rechtfertigen. Veränderungen der Kopfhaut, wie Trockenheit, können die Haargesundheit beeinträchtigen.

Diese Haut- und Haarveränderungen sind nicht nur Eitelkeitsprobleme; sie sind Signale deines Körpers über innere Veränderungen. Der Schlüssel liegt darin, mit sanfter, unterstützender Pflege zu reagieren, anstatt mit aggressiven Produkten oder das Problem zu ignorieren:
-
Hydratisiere und nähre deine Haut: Wechsle zu sanfteren, nicht austrocknenden Reinigungsmitteln, die deine Haut nicht austrocknen. Nach der Reinigung trage reichhaltige Feuchtigkeitscremes oder Gesichtsöle auf, während deine Haut noch feucht ist, um die Feuchtigkeit einzuschließen. Achte auf Inhaltsstoffe wie Ceramide, Hyaluronsäure und Glycerin, die dabei helfen, die Feuchtigkeitsbarriere der Haut aufrechtzuerhalten. Für zusätzliche Unterstützung können Gesichtsöle mit Inhaltsstoffen wie Hagebuttenöl oder Nachtkerzenöl essentielle Fettsäuren liefern, die die Haut nähren.
-
Schütze und stimuliere Kollagen: Konsequenter Sonnenschutz ist entscheidend – verwende tagsüber immer Sonnenschutz, da UV-Strahlung den Kollagenabbau beschleunigt und Pigmentierung verursacht. Nachts können sanfte Optionen wie Bakuchiol (eine pflanzliche Alternative) hilfreich sein.
-
Unterstütze die Haut von innen: Ausreichende Flüssigkeitszufuhr (erinnerst du dich an unsere Diskussion über Hydratation!) verbessert die Prallheit der Haut. Eine abwechslungsreiche Ernährung reich an Vitaminen und Antioxidantien (aus Obst und Gemüse) plus gesunde Fette (wie Omega-3-Fettsäuren in Fisch, Walnüssen, Leinsamen) unterstützt die Hautgesundheit. Diese Nährstoffe helfen dabei, Entzündungen zu reduzieren und Bausteine für gesunde Haut und Haare zu liefern.
-
Haarpflege-Anpassungen: Verwende ein sanftes Shampoo, um Trockenheit zu bekämpfen. Vermeide sehr straffe Frisuren oder aggressive chemische Behandlungen, die dünner werdendes Haar zusätzlich belasten können. Manche Frauen stellen fest, dass die Einnahme von Nahrungsergänzungsmitteln wie Biotin oder Kollagen oder die Sicherstellung einer ausreichenden Eisen- und Vitamin-D-Zufuhr bei der Haarstärke hilft – aber es ist ratsam, vor der Einnahme von Nahrungsergänzungsmitteln einen Arzt oder eine Ärztin zu konsultieren.
Insgesamt solltest du Haut- und Haarveränderungen mit Geduld und Selbstfürsorge begegnen. Diese Veränderungen sind Botschaften, dass dein Körper in diesen Bereichen zusätzliche Unterstützung braucht. Durch die Anpassung deiner Hautpflegeroutine und möglicherweise deiner Ernährung oder Nahrungsergänzungsmittel kannst du verbessern, wie sich deine Haut anfühlt und aussieht. Und denke daran: Jede Falte oder jedes graue Haar erzählt auch eine Geschichte – sie sind Teil deiner Reise. Die Pflege deiner Haut und Haare hilft dir dabei, dich wohl und selbstbewusst zu fühlen, aber die natürlichen Veränderungen mit Selbstmitgefühl zu akzeptieren ist genauso wichtig.
Körperliche und emotionale Veränderungen: Nach innen beobachten
Die Lebensmitte bringt eine Vielzahl körperlicher und emotionaler Veränderungen mit sich, die die Gesundheit und Lebensqualität von Frauen beeinträchtigen können. Emotionale Veränderungen während der Lebensmitte, besonders in der Perimenopause und Menopause, fühlen sich oft unvorhersagbar und intensiv an.
Reizbarkeit, Angst, Traurigkeit, erhöhte Stressreaktivität und sogar Depressionen können ohne klare äußere Ursache auftreten und manchmal schnell wechseln. Diese Gefühle sind keine Zeichen von Schwäche; sie entstehen oft aus dem komplexen Zusammenspiel zwischen schwankenden Hormonspiegeln und der Gehirnchemie. Östrogen beeinflusst die Aktivität von Neurotransmittern wie Serotonin, Dopamin und Norepinephrin, wichtigen Regulatoren für Stimmung, Motivation und Stressreaktion. Wenn die Östrogenspiegel schwanken und abnehmen, können diese Systeme beeinträchtigt werden, was zu Stimmungsinstabilität führt. Progesteron hat ebenfalls beruhigende Wirkungen, und sein Rückgang trägt zu verstärkter Angst bei.
Über die direkten hormonellen Auswirkungen hinaus spielt die Darm-Hirn-Achse eine bedeutende Rolle. Hormonelle Veränderungen können das Gleichgewicht des Darmmikrobioms stören; dieses Ungleichgewicht beeinflusst die Stimmung, indem es die Produktion von Neurotransmittern und Entzündungsmarkern beeinträchtigt.

Während Therapie Unterstützung bietet, sind auch Anpassungen des Lebensstils kraftvolle Werkzeuge.
Alltägliche Strategien, die helfen können, deine Stimmung zu stabilisieren und zu heben:
-
Suche morgendliches Licht: Ausreichend natürliches Licht zu bekommen, besonders am Morgen, hilft dabei, deinen zirkadianen Rhythmus zu regulieren und kann deine Stimmung und Energie verbessern. Versuche, für einen kurzen Spaziergang nach draußen zu gehen oder zumindest als erstes am Morgen die Vorhänge zu öffnen.
-
Halte eine Routine ein: Unsere Körper und unser Geist finden Sicherheit in Routinen. Versuche, regelmäßige Zeiten für das Aufwachen, Mahlzeiten, Sport und Schlaf einzuhalten. Ein konstanter Tagesrhythmus kann dabei helfen, deine innere Uhr und Hormonausschüttungsmuster auszugleichen, was Stimmungsschwankungen lindern kann.
-
Begrenze Überstimulation: Wenn du merkst, dass du leichter überwältigt oder reizbar bist, erwäge, übermäßigen Lärm oder Informationen in deiner Umgebung zu reduzieren. Das könnte bedeuten, Grenzen bei der Exposition gegenüber stressigen Nachrichten zu setzen, dir täglich etwas ruhige Zeit zu verschaffen oder einen hektischen Zeitplan zu vereinfachen, wo möglich. Ein ruhigeres Nervensystem neigt weniger dazu, in Angst oder Reizbarkeit zu verfallen.
-
Achtsamkeit und Stressreduktion: Praktiken wie Meditation, tiefe Atemübungen oder sanftes Yoga können helfen, deinen Geist zu zentrieren. Sogar kurze Achtsamkeitspausen während alltäglicher Aufgaben – wie sich auf das Gefühl warmen Wassers an den Händen beim Geschirrspülen zu konzentrieren – können Inseln der Ruhe schaffen. Mit der Zeit summieren sich diese kleinen Momente der Achtsamkeit und können deine allgemeine Widerstandsfähigkeit gegen Stress erhöhen.
-
Kreative Ausdrucksmöglichkeiten: Sich mit Hobbys oder kreativen Aktivitäten zu beschäftigen (wie Zeichnen, Schreiben, Musik oder Gartenarbeit) bietet ein positives Ventil für Emotionen. Kreativität kann therapeutisch sein und gibt dir eine Pause von alltäglichen Stressoren, was dabei hilft, deine Stimmung zu heben.
Vor allem praktiziere Selbstmitgefühl. Erinnere dich daran, dass Stimmungsschwankungen oder Angst während der Lebensmitte häufig sind und oft physiologisch bedingt. Es ist kein persönliches Versagen. Wenn du emotional einen schlechten Tag hast, behandle dich selbst mit der gleichen Freundlichkeit, die du einem guten Freund entgegenbringen würdest. Indem du mentale Gesundheit und Selbstfürsorge priorisierst – sei es ein entspannendes Bad, Zeit mit Liebsten oder ein Gespräch mit einem Therapeuten – baust du emotionale Widerstandsfähigkeit auf. Das hilft dir dabei, einen gesunden, aktiven Lebensstil während der Wechseljahre und darüber hinaus aufrechtzuerhalten, auch angesichts hormoneller Turbulenzen.
Verdauungsveränderungen: Der vergessene Rückkopplungskreislauf
Das Magen-Darm-System ist hochsensibel für hormonelle Schwankungen; Veränderungen der Verdauung sind häufige, aber oft übersehene Symptome der Wechseljahre. Östrogen beeinflusst die Darmbeweglichkeit, die Darmschleimhaut und die Zusammensetzung/Vielfalt des Darmmikrobioms.
Mit dem Rückgang des Östrogens berichten viele Frauen in der Lebensmitte über neue oder sich verschlimmernde Verdauungsprobleme wie Blähungen, Völlegefühl, Unregelmäßigkeiten (Verstopfung oder manchmal Durchfall) und Nahrungsmittelunverträglichkeiten. Reduziertes Östrogen kann die Darmbeweglichkeit verlangsamen, wodurch das Essen länger im Verdauungstrakt verweilt, was Verstopfung verursacht und Blähungen sowie Völlegefühl verstärkt. Veränderungen des Östrogens wirken sich auch auf das Darmmikrobiom aus. Ein Rückgang kann das Bakteriengleichgewicht verändern und möglicherweise zu Dysbiose führen, was zu Entzündungen und Verdauungsbeschwerden beiträgt.
Darüber hinaus erhält Östrogen die Integrität der Darmschleimhaut aufrecht. Sein Rückgang kann die Darmdurchlässigkeit erhöhen ("durchlässiger Darm"), wodurch Partikel in den Blutkreislauf gelangen und möglicherweise Immunreaktionen und Entzündungen auslösen. Das Darmmikrobiom beeinflusst, wie Hormone verstoffwechselt und ausgeschieden werden, wodurch eine Wechselwirkung entsteht, bei der hormonelle Veränderungen den Darm beeinflussen und die Darmgesundheit das Hormongleichgewicht beeinflusst.
Du könntest feststellen, dass sich Mahlzeiten schwerer anfühlen oder bestimmte Zutaten plötzlich entzündungsfördernd wirken. Darauf zu achten, wie du dich 30 Minuten bis einige Stunden nach dem Essen fühlst, liefert wertvolles Feedback.

Strategien zur Unterstützung der Verdauung in der Lebensmitte:
Konzentriere dich darauf, das Darmmikrobiom und eine gesunde Darmfunktion zu fördern.
-
Fokus auf Ballaststoffe: Essentiell für die Ernährung nützlicher Bakterien und die Förderung gesunder Darmbewegungen.
-
Fermentierte Lebensmittel einbauen: Probiotikareiche Lebensmittel helfen dabei, nützliche Bakterien einzuführen.
-
Gesunde Fette priorisieren: Omega-3-Fettsäuren reduzieren Entzündungen.
-
Achtsames Essen: Kleinere Mahlzeiten, gründliches Kauen und langsames Essen verbessert die Verdauung.
-
Flüssigkeitszufuhr: Entscheidend für die Vorbeugung von Verstopfung.
-
Bitterkräuter: Traditionell verwendet zur Unterstützung der Leber- und Gallenfunktion, was die Fettverdauung unterstützt.
-
Nährstoffaufnahme fördern: Veränderungen können die Aufnahme wichtiger Nährstoffe beeinträchtigen. Die Unterstützung der Verdauung optimiert die Nährstoffaufnahme.
Die Verdauung in der Lebensmitte profitiert von einem sanfteren, achtsameren Ansatz, der die erhöhte Empfindlichkeit und die wichtige Verbindung zwischen Darmgesundheit und allgemeinem Wohlbefinden anerkennt.
Jenseits des Körperlichen: Das Flüstern der Identität
Während sich der Körper verändert, wandelt sich auch das Selbstverständnis. Die Lebensmitte fällt oft mit wichtigen Lebensübergängen zusammen – Kinder verlassen das Zuhause, die Pflege alternder Eltern, berufliche Veränderungen, Beziehungswandel und eine Neubewertung der Werte. Alte Annahmen darüber, wer du bist, können sich auflösen. Das sind nicht nur äußere Ereignisse; sie hallen innerlich nach und regen zur Selbstreflexion und potentiellen Neuerfindung an.
Hier zu lauschen erfordert Übung und Mut. Es bedeutet zu bemerken, was nicht mehr passt – Rollen, Beziehungen oder Selbstkonzepte. Das beinhaltet, um vergangene Identitäten zu trauern, öffnet aber auch Raum für neue Möglichkeiten und Selbstentdeckung. Auf diese Ebene zu achten ist genauso wichtig wie körperliche Symptome zu verfolgen.
Bewussten Raum für Selbstreflexion zu schaffen ist der Schlüssel. Meditation hilft dabei, das gedankliche Gedränge zu beruhigen. Kreativer Ausdruck verarbeitet innere Veränderungen. Zeit in der Natur bietet Perspektive und Erdung. Aktivitäten, die äußere Anforderungen verlangsamen und inneres Lauschen ermöglichen, sind von unschätzbarem Wert.

Spiritualität, sei es durch Glauben oder Reflexion, vertieft sich oft. Fragen verschieben sich von äußeren Errungenschaften hin zur Erforschung der inneren Landschaft und des Lebenszwecks. Das ist ein wesentlicher Teil des Zuhörens, bei dem innere Wahrheit mit äußeren Entscheidungen in Einklang gebracht wird. Diese Phase als Gelegenheit für Wachstum zu begreifen, verwandelt die Lebensmitte in ein kraftvolles Kapitel authentischen Lebens.
Den Übergang der Wechseljahre meistern
Das erfolgreiche Meistern des Übergangs der Wechseljahre erfordert einen ganzheitlichen Ansatz, der sowohl unmittelbare Symptome als auch langfristige Gesundheit angeht. Gesundheitsdienste für Frauen in der Lebensmitte umfassen oft Hormonersatztherapie, Beratung und Aufklärung über gesunde Lebensgewohnheiten wie ausgewogene Ernährung, regelmäßige Bewegung und effektives Stressmanagement.
Veränderungen in der Lebensmitte stellen, anstatt einen Niedergang zu bedeuten, eine Einladung dar, tiefer auf die Intelligenz des Körpers zu hören. Jedes Signal ist Kommunikation eines sich anpassenden Körpers. Durchdacht zu reagieren, mit Neugier statt Kritik, mit Mitgefühl statt Frustration, unterstützt Vitalität, Würde und Wohlbefinden.
Letztendlich ist das Ziel nicht, perfekte Kontrolle zu haben oder sich wieder wie 21 zu fühlen. Es geht darum, eine tiefere Verbindung zu deinem Körper aufzubauen, während er sich verändert, seine Bedürfnisse zu verstehen und nachhaltig für ihn zu sorgen. Das bedeutet, eine Partnerschaft mit deinem Körper zu kultivieren – seine Weisheit und Signale zu respektieren und ihn mit dem gleichen Mitgefühl zu pflegen, das du einer engen Freundin entgegenbringen würdest. Das Gespräch mit deinem Körper ist fortlaufend und entwickelt sich weiter. Indem du auf seine Weisheitsflüstern hörst und mit unterstützenden Entscheidungen reagierst, kannst du dich in ein erfülltes, gesundes nächstes Lebenskapitel führen.
FAQ
Was sind die ersten Anzeichen der Wechseljahre?
Die Wechseljahre Symptome beginnen meist schleichend während der Perimenopause mit Hitzewallungen und nächtlichen Schweißausbrüchen, Schlafstörungen (oft Aufwachen um 3 Uhr morgens), Stimmungsschwankungen, Scheidentrockenheit und Veränderungen der Schleimhäute. Viele Frauen bemerken auch Verdauungsveränderungen, dass Speisen schwerer verdaulich werden und die Erholung länger dauert.
Welche 4 Phasen der Wechseljahre gibt es?
Der Artikel erwähnt hauptsächlich die Perimenopause als zentralen Übergang mit schwankenden Hormonen, die sich typischerweise über die 40er und 50er Jahre erstreckt. Die Menopause wird als ein Jahr nach der letzten Regelblutung definiert. Weitere spezifische Phasen werden im Artikel nicht detailliert beschrieben.
Welche Phase der Wechseljahre ist die schlimmste?
Laut dem Artikel ist die Perimenopause besonders herausfordernd, da Frauen in den Wechseljahren während dieser Phase intensive Wechseljahresbeschwerden erleben: Hitzewallungen und Schweißausbrüche, Schlafprobleme, Stimmungsschwankungen und Schmerzen beim Geschlechtsverkehr. Die Frauenärztin Dr. Brown betont, dass diese Symptome der Wechseljahre tiefgreifende Botschaften eines Körpers in natürlicher Umstellung sind.
In welchem Alter beginnen die Wechseljahre?
Der Artikel gibt an, dass sich die Perimenopause typischerweise über die 40er und 50er Jahre einer Frau erstreckt und bedeutende hormonelle Veränderungen mit sich bringt, die nahezu jedes Körpersystem beeinflussen. Ein spezifisches Alter für den Beginn der Wechseljahre wird nicht genannt.













